How Is A Displaced Caterach Lens Repaired
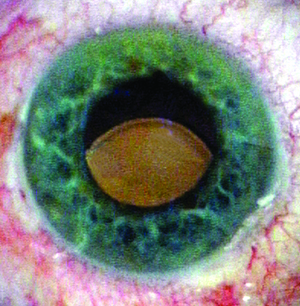 |
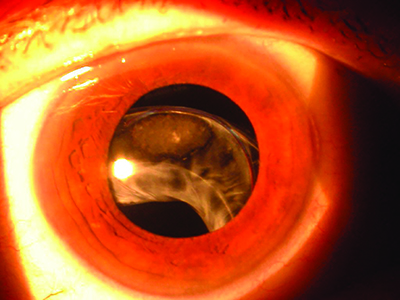
| Figure 1. Sunsetting three-piece IOL placed in the ciliary sulcus. (All images courtesy Richard Hoffman, MD.) |
Most cataract procedures are performed with no complications. The IOL is placed securely in the capsular bag, and information technology stays there for the duration of the patient'south life. Nevertheless, in some cases, the IOL can become dislocated to the point where a secondary intervention is required. In this article, expert surgeons share the techniques they employ when faced with a dislocated lens.
The Scope of the Trouble
According to Richard Hoffman, MD, who is in practice in Eugene, Oregon, IOL dislocations can be divided into five categories:
• A lens that's decentered within an intact capsular pocketbook.
• An IOL that's partially
• A lens that'due south in the sulcus, and then there is a compromised capsular pocketbook. The lens is in the sulcus, and that lens is decentered.
• An IOL that's in the capsular bag, and both are
• An IOL that's completely dislocated and is sitting on the retina.
"Each of these can be approached using multiple techniques, so there isn't one best technique for all scenarios," Dr. Hoffman explains.
Uday Devgan, MD, who is in practice in Los Angeles and a professor at UCLA, notes that the operative report from the original cataract surgery can assistance determine whether there were complications. "Determine if the IOL was placed in the capsular bag, or perhaps in the ciliary sulcus. Loose zonules may take been noted during the original procedure. Was the case uneventful or was there a posterior-sheathing rupture? Finally, annotation which type of IOL was placed and its dioptric power," he says. Videos of how to manage dislocated IOLs tin can be seen on Dr. Devgan's website: cataractcoach.com.
Decentered IOL in the Bag
Some IOLs are decentered merely nevertheless in the bag. This tin occur spontaneously or every bit a outcome of trauma.
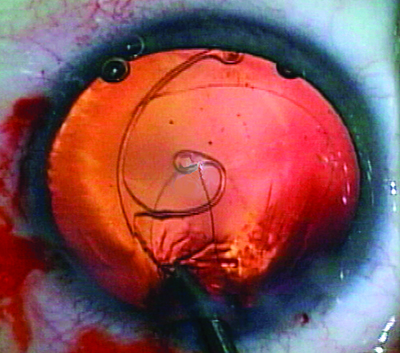 |
| Effigy 2. Ahmed segment with 9-0 Prolene suture beingness placed in the capsular bag following cataract extraction. |
"The classic case of this is pseudoexfoliation syndrome," says Alan Crandall, Doctor, senior vice-chair of Ophthalmology and Visual Sciences, and director of
For a decentered IOL within an intact capsular handbag, Dr. Hoffman says the all-time approach is to
Partially Subluxed IOL
If an IOL is partially in the capsular handbag and partially out of the capsular purse, Dr. Hoffman says he would
An IOL in the Sulcus
If a iii-slice lens is placed in the sulcus without any type of fixation, the lens will stay centered most of the time. On occasion, the IOL will work its style through the zonules and become decentered. "For these lenses, I will iris-fixate them with 9-0 or ten-0 Prolene," Dr. Hoffman explains.
He adds that direction also depends on the presentation and type of IOL. If there'due south a single-piece lens in the sulcus, information technology typically needs to be replaced with a iii-piece lens. "For patients with
Decentered IOL and Bag
In-the-handbag posterior chamber IOL dislocations can be managed by exchange with an inductive chamber IOL or past repositioning the posterior chamber IOL. 1
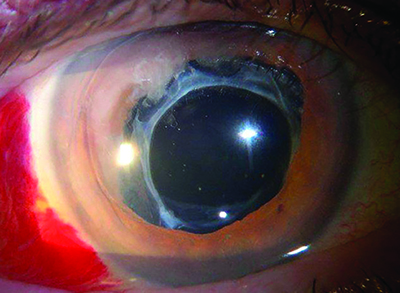 |
| Effigy 3. IOL with capsular tension ring |
For the scenario in which the IOL is in the capsular bag and the whole bag has come loose and
In these cases, the lens does well for 12 to 14 years after routine cataract
Dr. Crandall notes that his treatment of pick depends on the IOL that has been implanted and the patient's vision before surgery. "If the patient's vision was good, the IOL is not damaged and the handbag is intact or has a capsular tension band, I would identify the optic-haptic junction either intraoperatively or preoperatively," he explains. "I would and then mark 180 degrees from that, open upward the conjunctiva, clear off dorsum to 3 to 4 mm posterior, so find the surgical limbus and go two mm posterior to that and brand an incision into the sclera," he explains.
Then, he makes a lasso, lassoes the lens and the secures it to the sclera with 8-0 Gore-Tex, which is an off-label utilise, or with 9-0 or ten-0 Prolene sutures. He notes that there are a few different means to accomplish this. One instance is an ab
Garry Condon, Doc, professor of ophthalmology at the Drexel Academy Higher of Medicine, Allegheny Programme, in Pittsburgh, Pennsylvania, has described a simplified modification to the ab
A description of Dr. Condon's technique: Under anesthesia, he creates a
 |
| Effigy 4. Pseudophakic middle with |
The surgeon then uses Precipitous Westcott scissors to create a 3-mm vertically oriented, temporal, conjunctival and Tenon'southward sheathing dissection two mm posterior to the limbus. Then, a diamond bract is used to create a three-mm, ane-third-thickness scleral groove ii mm posterior to the limbus. Next, at i terminate of the fractional-thickness groove, a single 1-mm,
The surgeon then passes a ix-0 polypropylene double-armed suture on a long curved needle (D8229, Ethicon) through the margin of the partial-thickness scleral groove contrary the stab incision, up through the optic-haptic portion of the IOL-capsular bag circuitous, and out the peripheral cornea. If the needle won't laissez passer hands through the complex, the surgeon tin can apply counter traction with an intraocular microforceps to ensure successful passage of the needle. Then, a 30-caste iris hook is passed through the total-thickness scleral incision to recollect the polypropylene suture inductive to the posterior capsule IOL-capsular pocketbook complex.
The surgeon and so cuts the needle so the suture can be tied at the scleral groove. To allow subsequent IOL centration, a slipknot is placed, and the same process is repeated at the nasal aspect to secure the fellow optic-haptic portion of the IOL-capsular bag complex. The nasal polypropylene suture needle pass and ane-mm stab incision for suture retrieval counter the temporal sites to forbid IOL tilt. The surgeon adjusts the suture tension on both haptics to centre the IOL before securing and burial the knots. A single buried 8-0 polyglactin suture is used to close the conjunctiva. Too, express 23-guess pars plana vitrectomy either early on or at the conclusion of fixation may exist necessary, depending on the extent of vitreous involvement with the dislocated IOL-capsular bag complex.
According to Dr. Crandall, another option is to go underneath, the same style as described above, simply then dock the lens with a 26- or 27-ga needle inserted through a stab incision 180 degrees away. "Then, you pull that out and reverse information technology," he says. "This fourth dimension, you go above the bag and simply exterior. Both options are piece of cake and fast, and they work very well. So, you've secured the IOL complex."
However, if the patient's preoperative vision wasn't good or the lens is damaged, the surgeon may need to do a lens replacement. "If it's an older PMMA lens, then you must brand an incision that'due south at to the lowest degree 5, 5.5, or maybe half dozen mm depending on the implant," Dr. Crandall advises. "Once the old lens has been removed, you tin can implant a lens like the Alcon CZ70BD, which is a large PMMA lens that has eyelets on information technology. You just put the lens in, and you've already got sutures through the eyelets. You pull them out posterior to the limbus. In this case, you've obviously made a large incision that will require sutures. It works well, merely it's not the preferred technique because these optics ordinarily have some other problems, and you lot're risking glaucoma, infections, et cetera."
IOL Lying on the Retina
In cases where the IOL is completely dislocated onto the retina, Dr. Hoffman coordinates with a retina specialist. "If it was a iii-piece lens, the retina specialist would exercise a vitrectomy and pull the lens up, and then I would iris-fixate it," he says. "Simply, I don't do that anymore because
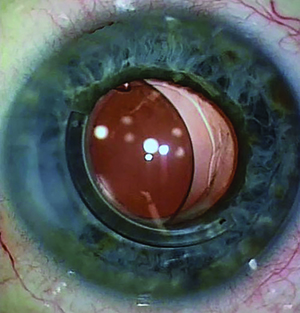
 |
| Figure v. Subluxed IOL/capsular bag/capsular tension ring in a patient with pseudoexfoliation. |
The lens tends to movement effectually a lot and sometimes causes chronic hyphemas or uveitis. And so, in those situations, I now accept the retina surgeon bring the lens up into the anterior sleeping accommodation, and then I remove the lens. So, I will scleral-fixate a new lens using a scleral incarceration technique. The latest one is the Yamane technique." 1. Gross JG, Kokame GT, Weinberg DV; Confused in-the-bag intraocular lens study group. In-the-pocketbook intraocular lens dislocation. Am J Ophthalmol 2004;137:4:630-635.
The Yamane technique for transconjunctival
Preoperatively, the mean best-corrected visual acuity was 0.25 logMAR units (around 20/35 Snellen), which significantly improved postoperatively to 0.11 (slightly worse than 20/25) at six months, 0.09 (slightly worse than 20/24) at 12 months, 0.12 (20/26) at 24 months, and 0.04 (slightly worse than 20/20) at 36 months.
Mean corneal endothelial cell density decreased from 2,341 cells/mm 2 preoperatively to 2,313 cells/mm 2 , 2,240 cells/mm ii , two,189 cells/mm2 and 2,244 cells/mm 2 postoperatively at six, 12, 24, and 36 months, respectively, and hateful IOL tilt was 3.four ±ii.v degrees. Postoperative complications included iris capture by the IOL in eight eyes (8 percent), vitreous hemorrhage in five optics (v pct), and cystoid macular edema in one eye (i percent). No patients experienced postoperative retinal detachment, endophthalmitis or IOL dislocation.
According to Dr. Crandall, the surgeon should apply any technique he is comfy with. "If yous have non performed some of these techniques, I call back it's a good idea to watch some other surgeon exercise them in person and non just on YouTube, because many subtleties of the techniques are edited out. Many of these subtleties can brand the surgery much easier," he adds. REVIEW
three. Kirk TQ, Condon GP. Simplified ab
iv. Yamane S, Sato South, Maruyama-Inoue M, Kadonosono Chiliad. Flanged
Source: https://www.reviewofophthalmology.com/article/how-to-manage-dislocated-iols
Posted by: dahmsfuriall.blogspot.com


0 Response to "How Is A Displaced Caterach Lens Repaired"
Post a Comment